Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Hypercholesterolaemia contributes to a higher risk of cardiovascular diseases, such as heart disease and stroke, and it is estimated that more than 20 million people in England have elevated cholesterol levels.1
Globally, a third of ischaemic heart disease is attributable to high cholesterol and this accounts for 7.1% of deaths and 3.7% of disability-adjusted life years in England. It is also estimated that 145,000 heart attacks, strokes and premature deaths could be prevented over the next decade if people’s cholesterol levels were lowered.2
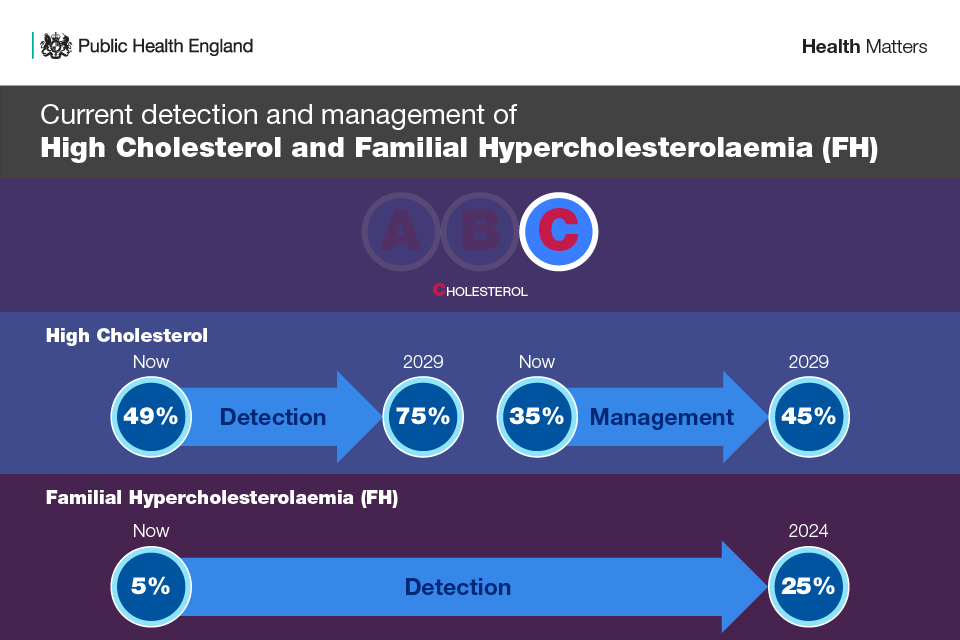
For this reason, lipid lowering is one of the high-risk conditions that form part of the NHS Long Term Plan ‘ABC’ (Atrial Fibrillation, Blood Pressure and Cholesterol) ambitions.2
This aims to support local NHS teams in detection and management of cholesterol lowering through monitoring and targeting unwarranted variation, supporting a system-wide response, and increasing public education.
Primary prevention of cardiovascular disease
Atherosclerosis is a condition where there is a build-up of fatty deposits (plaques) inside an artery. This is made up of deposits of fatty substances, cholesterol, cellular waste products, calcium, and fibrin. It can cause the artery to harden and narrow, restricting blood flow. Cardiovascular conditions caused by atherosclerosis include:
-
- Coronary heart disease (including angina and myocardial infarction).
- Stroke.
- Transient ischaemic attack (TIA).
- Peripheral arterial disease.3
The identification of people with, or at risk of developing, CVD is essential to allow timely intervention to reduce their cholesterol level and minimise their risk of heart attack or stroke.4
One of the aims of the cholesterol ambition is for 75% of eligible people aged 40 to 74 without established CVD to have a CVD risk assessment and cholesterol reading recorded by 2029.
This includes baseline blood tests and a clinical assessment. NICE guidance recommends taking a blood sample to measure total cholesterol, HDL cholesterol and triglyceride levels and then calculating non-HDL cholesterol and LDL cholesterol.
It also recommends excluding possible secondary causes of dyslipidaemia (such as excess alcohol, uncontrolled diabetes, hypothyroidism, liver disease and nephrotic syndrome).
A family history should also be taken to judge the likelihood of a familial lipid disorder, rather than using strict lipid cut-off values alone. Familial hypercholesterolemia (FH) is an inherited condition that results in high levels of blood cholesterol and a high risk of heart disease at an early age. Management of FH with lipid-lowering therapy, such as statins, is highly effective but most people with FH are undetected and therefore not managed.2
The estimated prevalence is 1 in 500, suggesting 120,000 affected individuals in Britain, but with only 15-17% of cases identified in the UK.5 This is why the NHS has set an ambition for 25% of the expected number of people with FH to be genetically identified and optimally managed.2
Lifestyle modifications
In recent years, with the boom of the wellness sector, there has been a growth in more holistic ways to lower cholesterol, which include exercise, reducing alcohol and stopping smoking.
Dietary management of lipid lowering is constantly evolving with current research showing that for most healthy people, cholesterol in food, such as eggs, has a much smaller effect on blood levels of total cholesterol and harmful LDL cholesterol. Instead, the American Heart Association recommends limiting dietary saturated fat intake and focusing more on eating fruits, veggies, whole grains, lean animal protein or plant protein sources.6
This is why it is important that before treatment options, healthcare professionals discuss the benefit of lifestyle modifications and optimise the management of all other modifiable CVD risk factors, including any relevant comorbidities that may not be optimally treated.
Then patients should be offered the opportunity to reassess CVD risk again after they have tried to change their lifestyle.3
Physicians need to recognise that some people may need support to change their lifestyle — to help, refer them to programmes such as exercise referral schemes or smoking cessation services.
Statins
Monitoring of cholesterol levels usually takes place in primary care and the decision to prescribe an additional treatment will be taken by a GP and other primary care clinicians in discussion with the patient. Measures have been incorporated into the GP contractual framework to further expand the use of statins first line in people diagnosed with CVD.4
NICE recommends that statins should be offered to people who have a 10% or greater 10-year risk of developing CVD. For some people, it may be necessary to start statin therapy straight away.3
Statins have been first-line therapy for lowering cholesterol for over three decades. Even though they are one of the most prescribed drugs in the UK, with an estimated 7-8 million adults taking them, there have been concerns around side effects, such as muscular aches and pains.
A recent BHF-funded research study however found that while statins are linked with a small increase in the risk of muscle pains or weakness, they don’t cause the majority of muscle pain symptoms commonly connected with them.7 NICE also says: “The best evidence shows that most people don’t get muscle pains with statins, and many more people will get muscle pains whether they take statins or not, than have muscle pain caused by statins.”
However, recent emerging evidence has suggested that statins confer increased risk of developing new-onset diabetes mellitus (NODM) It has been suggested that the risk of developing NODM during statin therapy is associated with statin intensity. In meta-analysis of data from 5 statin trials, high-intensity statin therapy more increased the incidence of NODM by 12% than moderate-intensity statin therapy.8
New treatments
In recent years, novel LDL-C lowering medications have been developed. Proprotein convertase subtilisin-kexin type 9 inhibitors (PCSK9i), such as alirocumab and evolocumab, reduce LDL-C by approximately 60%, reaching maximal reduction within four weeks at a similar safety profile to other interventions. PCSK9i have also been shown to reduce inflammation and progression of atherosclerotic disease.9
Other options include inclisiran, the small interfering ribonucleotide acid (si-RNA), as well as the recently approved bempedoic acid.10
Data from the phase III clinical studies of the ORION-10 and ORION-11 studies demonstrated that plasma levels of PCSK9 decrease by up to 80% after treatment initiation with inclisiran.10
In clinical trials, bempedoic acid on its own has been shown to reduce LDL cholesterol by between 17-28% after 12 weeks.11 When combined with ezetimibe, bempedoic acid can give up to 38% reduction in LDL cholesterol.
NICE guidance recommends that if statins alone are not sufficient to reach the blood cholesterol target in an individual, then clinicians can consider additional treatments, following a conversation on the risks and benefits with the patient.12
Secondary prevention
Updated final NICE guidance recently introduced a new target for cholesterol levels for people who have had a heart attack or stroke to reduce the risk of them having another.
The guidance recommends that for secondary prevention of CVD clinicians aim to keep patients’ LDL cholesterol levels at 2.0 mmol per litre or less, or non-HDL cholesterol levels of 2.6 mmol per litre or less.
It is estimated that by increasing the number of people reaching the 2.0 mmol per litre or less LDL target, many more health incidents can be avoided, including strokes, heart attacks, and premature deaths.
The potential benefits of implementing these recommendations will vary according to how many people with uncontrolled CVD take additional treatments to reduce their cholesterol. NICE estimates there could be between 50,000 and 145,000 fewer CVD events over 10 years.
References
- https://www.heartuk.org.uk/news/latest/post/168-aac-publishes-updated-clinical-pathway-for-lipid-management
- https://www.gov.uk/government/publications/health-matters-preventing-cardiovascular-disease/health-matters-preventing-cardiovascular-disease
- https://cks.nice.org.uk/topics/lipid-modification-cvd-prevention/
- https://www.england.nhs.uk/wp-content/uploads/2013/11/fh_eEngland-briefing11_2013.pdf
- https://www.england.nhs.uk/blog/cholesterol-awareness-month-driving-further-faster/
- https://health.clevelandclinic.org/why-you-should-no-longer-worry-about-cholesterol-in-food
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/behind-the-headlines/who-should-be-offered-statins
- Chung, J., Kim, HL., Lim, WH. et al. New onset diabetes mellitus and cardiovascular outcomes according to statin intensity in patients after drug-eluting stent implantation in Asian patients. Sci Rep 13, 16061 (2023). https://doi.org/10.1038/s41598-023-42277-w
- https://bjcardio.co.uk/2023/05/assessing-opinion-on-lower-ldl-cholesterol-lowering-and-the-role-of-newer-lipid-reducing-treatment-options/
- Burger AL, Pogran E, Muthspiel M, Kaufmann CC, Jäger B, Huber K. New Treatment Targets and Innovative Lipid-Lowering Therapies in Very-High-Risk Patients with Cardiovascular Disease. Biomedicines. 2022 Apr 22;10(5):970. doi: 10.3390/biomedicines10050970. PMID: 35625707; PMCID: PMC9138506.
- https://www.heartuk.org.uk/getting-treatment/bempedoic-acid
- https://www.nice.org.uk/guidance/NG238/history


