Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Up to 50% of men may experience pelvic pain or symptoms consistent with prostatitis in their lifetime, yet the condition is poorly understood and can be a challenge for physicians. In this first part in a new series, the authors look at classification and diagnosis of chronic prostatitis and chronic pelvic pain syndrome
Case study
NM, a 48 year old salesman presented to his GP with a one-year history of recurrent episodes of pain, felt in the perineum and at the tip of the penis during and for some time after passing urine. In addition, he experienced significant discomfort on ejaculation, and at times of more severe symptoms, increased urinary frequency and urgency. As a result of these symptoms, he was becoming increasingly low in mood – he also noticed that symptoms would often flare up during times of fatigue or stress.
Prostatitis is a common condition, with estimates of prevalence suggesting 35-50% of men experience symptoms consistent with the condition at some time in their life.1 Prostatitis is poorly understood, under- diagnosed and presents a diagnostic and therapeutic challenge for physicians.1 However, the condition has attracted relatively little attention from urologists (perhaps because it rarely requires surgical treatment) or the wider medical community when compared with other urological conditions, has often been presented as a ‘heartsink’ problem, and is under- represented in the medical literature. Prostatitis can have a huge detrimental impact on quality of life, 2 and is a cause of great frustration for patient and doctor due to the difficulty in understanding the condition and treating it successfully. However, if the symptoms are recognised and the diagnosis made, a symptom-based approach to treatment can be undertaken.
Classification of prostatitis
Presenting symptoms of prostatitis
Assessment and diagnosis in primary care
- NIH Chronic Prostatitis Symptom Index (NIH-CPSI) for general assessment of prostatitis symptoms
- International Prostate Symptom Score (IPSS) for quantification of urinary symptoms
- International Index of Erectile Function (IIEF-5) or Sexual Health Inventory for Men (SHIM) enable measurement of erectile function/sexual symptoms
- Patient Health Questionnaire-9 (PHQ-9) and/or the Generalised Anxiety Disorder-7 (GAD-7) for assessment of psychological impact of the condition, and can be used if a patient indicates that anxiety or mood issues have been a problem.
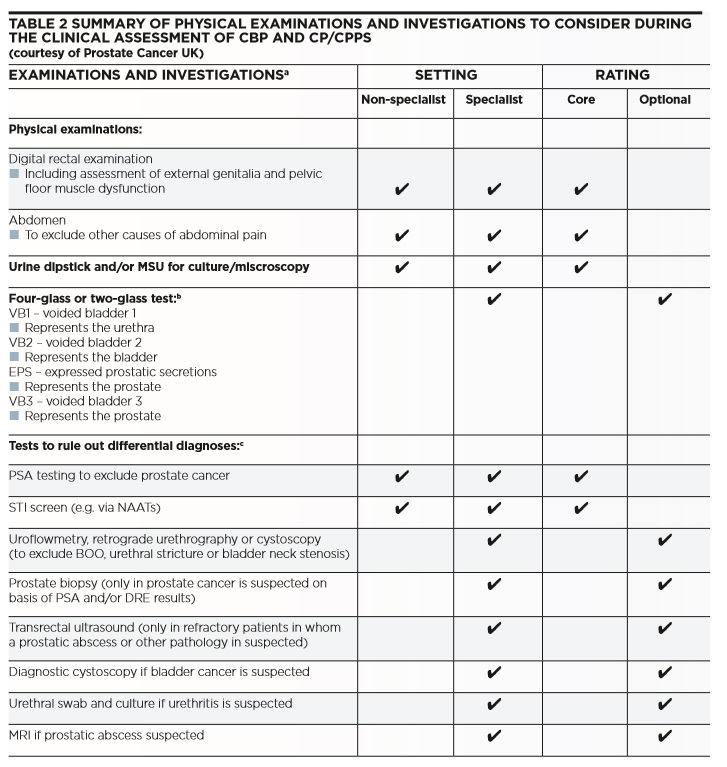
Examination of the patient should include a digital rectal examination (DRE), firstly to exclude abnormalities suggesting the possibility of prostate cancer which can occasionally present with pelvic pain, to estimate prostate size in the presence of urinary symptoms and to assess for excessive tenderness of the prostate and sometimes for pelvic floor issues, particularly hypertonicity. Only three key investigations need to be considered in primary care (see Table 2 ): urinalysis and microscopy if appropriate (in order to exclude urinary tract infection (UTI)), exclusion of sexually transmitted infection (particularly chlamydia) and discussion with the patient about the pros and cons of Prostate Specific Antigen (PSA) testing.4
This should be considered under the following circumstances: an abnormal prostate on DRE; patient concern in relation to prostate cancer; or when symptoms are suggestive of bladder outlet obstruction secondary to benign prostatic enlargement. While the PSA level can be falsely elevated during an infective or inflammatory flare of prostatitis, most men with pelvic pain and urinary symptoms are concerned about the possibility of prostate cancer. Therefore a baseline PSA test is often useful, if only hopefully for reassurance.
Dr Jonathan Rees GP with special interest in Urology, Backwell & Nailsea Medical Group
Dr Alison Cooper Prostate Cancer UK On behalf of the Prostatitis Expert Reference Group, Prostate Cancer UK
References
1 Pavone-Macaluso M. EAU-EBU Update Ser. 2007Feb;5(1):1–15.
2 McNaughton Collins M, Pontari MA, O’Leary MP, Calhoun EA, Santanna J, Landis JR, et al. J Gen Intern Med. 2001 Oct;16(10):656–62.
3 Nyberg L, Krieger J, Nickel J. National Institutes of Health Classification of Chronic Prostatitis. 1999.
4 Prostate Cancer UK. Diagnosis and treatment of chronic bacterial prostatitis and chronical prostatitis/chronic pelvic pain syndrome: a consensus guideline [Internet]. 2014. Available from: http://prostatecanceruk.org/prostatitisguideline
5 Wagenlehner FME, van Till JWO, Magri V, Perletti G, Houbiers JGA, Weidner W, et al. Eur Urol. 2013 May;63(5):953–9.
6 Clemens JQ, Meenan RT, O’Keeffe Rosetti MC, Gao SY, Calhoun EA. J Urol. 2005 Dec;174(6):2319–22.
7 Bartoletti R, Cai T, Mondaini N, Dinelli N, Pinzi N, Pavone C, et al. J Urol. 2007 Dec;178(6):2411–5; discussion 2415.
8 Anderson RU, Wise D, Sawyer T, Chan CA. J Urol. 2006 Oct;176(4 Pt 1):1534–8; discussion 1538–9.
9 Lee SWH, Liong ML, Yuen KH, Leong WS, Cheah PY, Khan NAK, et al. Urology. 2008 Jan;71(1):79–84.
10 Magri V, Perletti G, Montanari E, Marras E, Chiaffarino F, Parazzini F. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol Assoc Ric Urol. 2008 Dec;80(4):172–5.
11 Trinchieri A, Magri V, Cariani L, Bonamore R, Restelli A, Garlaschi MC, et al. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol Assoc Ric Urol. 2007 Jun;79(2):67–70.
12 Liang C-Z, Zhang X-J, Hao Z-Y, Shi H-Q, Wang K-X. BJU Int. 2004 Mar;93(4):568–70.
13 Davis SNP, Binik YM, Amsel R, Carrier S. J Urol. 2013 Jan;189(1):146–51.
14 Clemens JQ, Brown SO, Calhoun EA. J Urol. 2008 Oct;180(4):1378–82.
15 Anderson RU, Orenberg EK, Chan CA, Morey A, Flores V. J Urol. 2008 Mar;179(3):956–60.
16 Ku JH, Jeon YS, Kim ME, Lee NK, Park YH. Scand J Urol Nephrol. 2002;36(4):296–301.
17 Smith KB, Pukall CF, Tripp DA, Nickel JC. Arch Sex Behav. 2007 Apr;36(2):301–11.
18 Hedelin H. Scand J Urol Nephrol. 2012 Aug;46(4):273–8.
19 NHS Choices. Map of Medicine. Prostatitis – Primary Care [Internet]. 2014 [cited 2014 Jun 6]. Available from: http:// healthguides.mapofmedicine.com/choices/pdf/prostatitis1.pdf
20 NHS Choices. Map of Medicine. Prostatitis – Secondary Care [Internet]. 2014 [cited 2014 Jun 6]. Available from: http://healthguides.mapofmedicine.com/choices/pdf/prostatitis2.pdf
21 Nickel JC, Downey J, Clark J, Casey RW, Pommerville PJ, Barkin J, et al. Urology. 2003 Oct;62(4):614–7.


