Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Female genital mutilation (FGM) is an ancient practice dating back some 2,000 years to ancient Egypt and, although not explicitly mentioned is alluded to in the bible as a practice performed on Egyptian slaves. The practice of FGM is deeply embedded in certain communities and based on a range of motives, although the main reason relates to ensuring a woman is pure and chaste in preparation for marriage. FGM is prevalent in 28 African countries, parts of the Middle East and Asia (see Map). 1 FGM can lead to serious physical and psychological complications.
FGM is a form of abuse of women and children, illegal in the UK since the Female Circumcision Act of 1985, superseded by the Female Genital Mutilation Act of 2003, which extended the offence abroad and makes FGM punishable by up to 14 years in prison.2
With increasing migration, FGM is becoming more prevalent in the UK and clinicians need to be familiar with the issues and how to manage patients who have either undergone FGM or may be at risk of the practice. The Department of Health is gathering data regarding UK figures for FGM, although it is estimated that approximately 137,000 women and girls in England and Wales are survivors of FGM.3
This article looks at the background to FGM and aims to increase clinicians’ confidence in identifying and managing those who may be at risk of FGM or who have undergone this practice.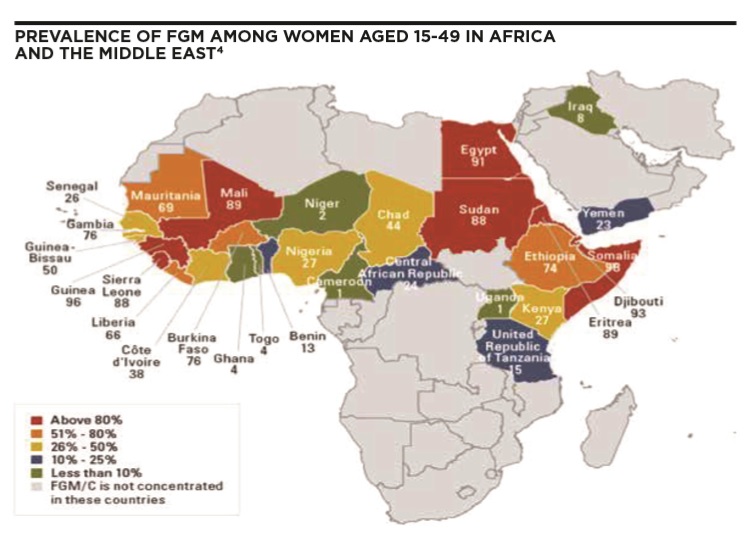
Motives for female genital mutilation
FGM is a practice deeply rooted in practising communities. Individuals rejecting FGM may be ostracised by their family and community. Motives for performing FGM vary between communities and reasons given can include:
- Aesthetics
- Purity
- Cleanliness
- Chastity
- As a rite of passage to womanhood
- To avoid harm to the baby at childbirth
- Social acceptance
- Respectability for the girl and her family
- Religious and cultural reasons. 4
Regarding religious reasons, there is no basis for the practice in religious texts of the Muslim, Christian or Jewish faiths.
Terminology
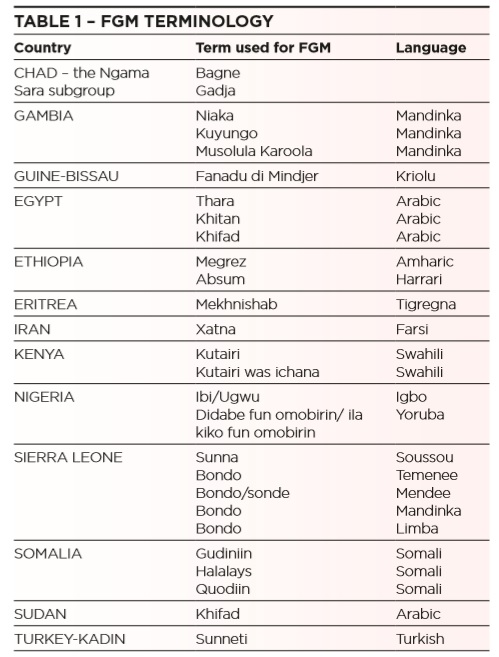
Female genital mutilation (FGM) is also known as female genital cutting and female circumcision. The term FGM is generally applied in professional literature and will be used in this article.
Notwithstanding this, it is important for clinicians to ensure that they employ the utmost sensitivity in the terminology they use when communicating with patients, as the term “mutilation” carries negative connotations that may impact on a patient’s self- esteem. Most would prefer to be referred to as “survivors” rather than “mutilated”.
Furthermore, patients may be unfamiliar with the term female genital mutilation and it would be preferable to refer to “cutting”, “female circumcision” or to use colloquial terms (see Table 1).
Definition
Female genital mutilation comprises all procedures involving the partial or total removal of the external female genitalia or other injury to the female genital organs for non-medical reasons. The practice entails the removal and/or damaging of normal female genital tissue and can interfere with the normal function of the female body.
FGM confers no health advantages and may lead to physical and psychological complications, and in the worst cases death of a female who has had FGM and/ or her child due to complications in pregnancy and/or labour as outlined below.
FGM may be performed at any age, though the peak prevalence appears to be 5-8 years of age. However, it is important to note that FGM may be undertaken on much younger girls, including newborns, and many patients may not be aware that they have undergone the procedure. Furthermore, women may undergo the procedure after childbirth in order to restore the narrow vaginal opening created by type 3 FGM and widened in childbirth. This is called reinfibulation.
FGM types
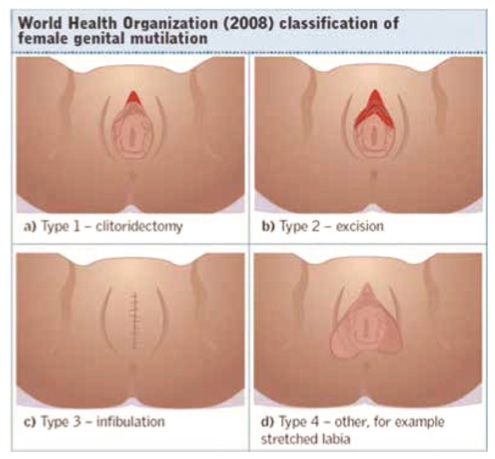
WHO has classified FGM into four types, and all are illegal in the UK. It may be difficult for a clinician to confidently diagnose the type of FGM performed, particularly in the case of type 4 FGM.
- Type 1: Clitoridectomy Partial or total excision of the clitoris, and in a few cases of the prepuce only.
- Type 2: Excision Partial or complete excision of the clitoris and labia minora, with or without the removal of the labia majora.
- Type 3: Infibulation Narrowing of the vaginal opening by forming a covering seal by cutting and repositioning the inner or outer labia. It may also involve removal of the clitoris. This is the most extreme physical type and tends to lead to the most physical complications for the woman or girl and at childbirth.
- Type 4: Other This type of FGM entails all other harmful practices to the female external genitalia for non-medical reasons, including pricking, piercing, incising, scraping and cauterising.5
Complications
In some areas, such as Egypt, the practice is more medicalised with the use of sterile equipment and anaesthetic, yet long term physical and psychological complications may still arise.
Clinicians should note that patients may be unaware that they have undergone FGM and, even if they are, may not associate FGM with some of the complications they may be experiencing.
Early physical complications:
- Death
- Damage to soft tissues, bones and organs due to being forcibly restrained
- Haemorrhage
- Extreme pain
- Infections, both local and systemic, including tetanus, hepatitis B and C, HIV
- Urinary retention.
Late physical complications:
- Complications in pregnancy and delayed second stage of labour particularly in type 3 FGM, which may lead to death of mother and child
- Obstetric fistulas
- Infections, including chronic and recurrent vaginal and pelvic infections, urine infections, systemic infections
- Difficulty passing urine, particularly in type 3 FGM
- Impaired renal function, including failure and chronic/recurrent UTIs
- Menstrual problems, including blockage of menstrual flow in type 3 FGM
- Infertility
- Dyspareunia and lack of pleasure during sexual intercourse
- Infibulation cysts, neuromas and keloid scarring locally.
Psychological complications
FGM is perceived by communities as an “act of love”, undertaken for the betterment of a girl’s life and to promote her acceptance into society as a chaste woman, in accordance with cultural precepts.
In the immediate aftermath of FGM, a woman or girl may be profoundly shocked by this practice having been arranged by loving parents and a caring community.
Scenarios
Consider the following case scenarios:
Case scenario 1
- A 20 year old Egyptian woman comes to see you complaining of a 3 day history of dysuria.
- She has been suffering with recurrent UTIs for the last 10 years.
- She appears anxious.
- She came to the UK with her family eight years ago and lives with her parents and two younger sisters.
Case scenario 2
- A 40-year-old mother of five, originally from Somalia, comes to see you about a flare up of her eczema.
- As you examine her skin she mentions that life at home is becoming increasingly difficult due to regular arguments with her husband.
- They don’t seem to agree on much lately and her husband wants to arrange a family trip to Somalia over the summer to visit relatives and friends. She is withdrawn and her mood appears low.
Case scenario 3
A school nurse contacts you to discuss her concerns regarding an 11 year old female pupil who has recently returned from a family trip to Ethiopia. She is spending long periods in the toilet and seems in some discomfort walking and sitting in class.
Case scenario 4
The practice nurse at your surgery comes to you with concerns regarding a young Nigerian woman she has just seen. She is three months pregnant but has not yet attended the surgery as she says she fears being examined and giving birth. Her sister’s labour lasted for three days, in which both her and her child nearly died.
Approach to management
Consider the probability of FGM bearing in mind the ethnic origin of these patients, the possible physical and psychological complications of FGM and how to manage these, as well as any risk to other females in the family and your safeguarding duties.
The 3 Cs questionnaire may assist when assessing whether FGM has been performed and to assess the risk of FGM:
- Do you come from a community that practices cutting?
- Have you, or a member of your family, been cut?
- Do you, or any member of your family or community, plan to get any female in your family cut?
A yes to at least one of these questions increases the risk of FGM and local safeguarding procedures should be followed.
If you do not ask the question, no-one will.
Women who have undergone FGM have comparable rates of PTSD as adults who have experienced abuse in early childhood, and 80% suffer from affective or anxiety disorders. 6
Psychological complications may include the following:
- Psychosexual problems, including sexual dysfunction and low libido
- Depression, including possible self-harm and substance misuse
- Anxiety
- PTSD
Risk factors for female genital mutilation
When considering a woman or girls risk of undergoing FGM, consider the following:
- Does she come from a practising community?
- Has any female member of her family had FGM, particularly her mother and sisters?
- How integrated is she and her family into UK society?
- Has she been removed from Personal, Social and Health Education to restrict her awareness of FGM? 4
Indicators of immediate risk of FGM:
- Planned visit “home” to see the family
- Mention of a special ceremony to mark entry to womanhood
- An older female relative visiting the UK
- Truancy
- Plea for help to a trusted adult outside of the community. 4
Signs female genital mutilation has been performed
A girl or woman may:
- Be in obvious discomfort
- Have difficulty walking, sitting or standing
- Spend long periods in the toilet due to problems urinating
- Spend long periods away from classes due to bladder or menstrual dysfunction
- Have frequent urinary, menstrual or abdominal symptoms, including pain
- Have prolonged or repeated absences from school
- Be particularly reluctant to undergo normal medical examinations, including smear tests and antenatal care
- Confide in a professional
- Ask for help, but not reveal details due to fear or embarrassment
- Experience pain between the legs.
Management
The GP’s role is:
- To manage physical and psychological consequences of FGM, including supporting survivors in coping with the consequences of FGM, and referral to secondary care and deinfibulation clinics where indicated
- To consider the risks to other females when a survivor of FGM has been identified
- To ensure those at risk are safeguarded from abuse.7
Regarding the physical consequences of FGM it may be necessary to refer a woman who has undergone the most extreme type of FGM, type 3, for deinfibulation, in order to widen the narrowed vaginal opening. Deinfibulation is a surgical procedure whereby the closed vaginal opening is opened.
With respect to safeguarding of children at risk of FGM, clinicians should promptly refer those at risk to social care, in accordance with safeguarding children principles and local policies and procedures.
Guidance relating to GPs dealing with cases of FGM: 8,9,10,11
- GPs must be familiar with guidelines and developments that affect your work
- GPs must keep up-to-date with, and follow, the law, our guidance and other regulations relevant to your work
- Under child protection guidance FGM is a safeguarding issue. GPs must report concerns that a child has suffered, or may be at risk of serious harm to an appropriate agency – such as the police, local authority children’s service or NSPCC – unless there are exceptional reasons for believing it would not be in the best interests of the child to do so. This applies to concerns about FGM
- You do not need to be certain that the child or young person is at risk of significant harm to take this step. If a child or young person is at risk of, or is suffering, abuse or neglect the potential consequences of not sharing relevant information will, in the vast majority of cases, outweigh any harm that sharing your concerns with an appropriate agency might cause
- GPs should develop an understanding of the practices and beliefs of different cultural and religious beliefs held by the local community
- In the case of adults, GMC guidance recognises the right of individuals who have capacity to make decisions in their own interests (including decisions about when their confidential information is disclosed), unless there is a public interest in overriding the person’s wishes or another legal basis for making a disclosure. Therefore, the GP should consult with the woman, about ways in which to proceed and should focus on supporting and empowering the woman to make decisions about disclosure of information about her. GPs should also encourage the woman to contact, or agree to disclosure to, services that can support her in dealing with the impact of FGM on her
- If a woman refuses consent for information to be shared, and that decision does not leave anyone else at risk of harm, GMC guidance advises that her decision should usually be respected. There can however be a public interest justification for sharing information about a woman without her consent if doing so would assist in the prevention, detection or prosecution of serious crime, or if failure to do so would leave others at risk of harm. 1
References
- Female genital mutilation and other harmful practices, WHO, http://www.who.int/reproductivehealth/topics/fgm/ prevalence/en/ (last accessed Jan 15)
- Female Genital Mutilation Legal Guidance, CPS, http://www.cps.gov.uk/legal/d_to_g/female_genital_mutilation/ (last accessed Jan 15)
- Female Genital Mutilation in England and Wales: Updated statistical estimates of the numbers of affected women living in England and Wales and girls at risk: Interim report on provisional estimates http://www.trustforlondon.org.uk/ wp-content/uploads/2014/07/FGM-statistics-report-21-07- 14-no-embargo.pdf (last accessed Jan 15)
- Multi-Agency Practice Guidelines: Female Genital Mutilation, Home Office, 2014 https://www.gov.uk/government/ uploads/system/uploads/attachment_data/file/380125/ MultiAgencyPracticeGuidelinesNov14.pdf (last accessed Jan 15)
- FGM guidance for professionals, NHS Choices, http://www. nhs.uk/NHSEngland/AboutNHSservices/sexual-health-services/ Pages/fgm-for-professionals.aspx (last accessed Jan 15)
- Mental problems and FGM, WHO, http://www.who.int/ reproductivehealth/topics/fgm/mental_problems_and_fgm/ en/ (last accessed Jan 15)
- Female Genital Mutilation resource pack, 2014 https://www. gov.uk/government/publications/female-genital-mutilation- resource-pack (last accessed Jan 15)
- Good medical practice, GMC, http://www.gmc-uk.org/ guidance/good_medical_practice.asp (last accessed Jan 15)
- Protecting children and young people: the responsibilities of all doctors, GMC http://www.gmc-uk.org/ publications/13683.asp (last accessed Jan 15)
- Confidentiality, GMC, http://www.gmc-uk.org/guidance/ ethical_guidance/confidentiality.asp (last accessed Jan 15)
- Introducing mandatory reporting for FGM, consultation. https://www.gov.uk/government/consultations/introducing- mandatory-reporting-for-fgm (last accessed Jan 15)
Dr Sharon Raymond MBBS MRCGP NHS London FGM Steering Group


