Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
One third (34%) of British adults are struggling to access healthcare services provided by the NHS, according to a survey by the Institute for Public Policy Research (IPPR).
The survey, which was published to coincide with the 75th anniversary of the NHS, found that this lack of access to healthcare is having an impact on people’s day-to-day lives, particularly those with a long-term illness.
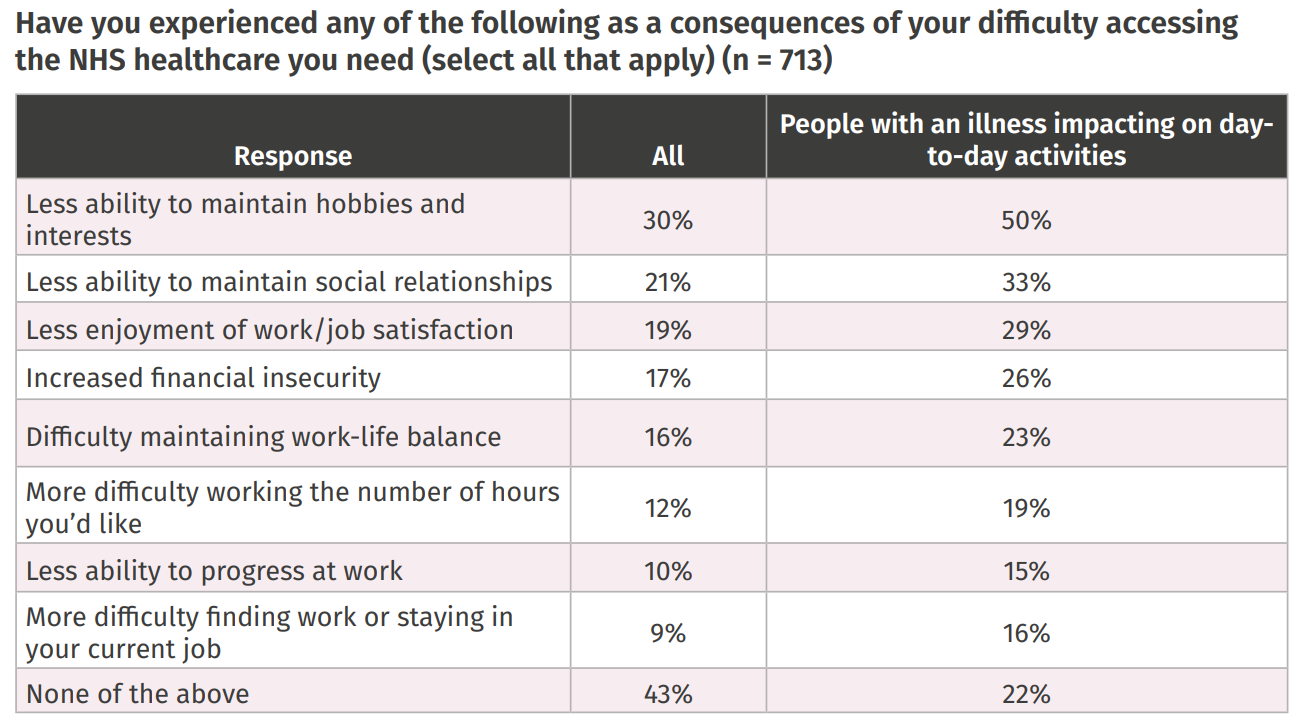
Indeed, half (50%) of people with an illness said they have less ability to maintain hobbies and interests, while a third (33%) said they struggle to maintain social relationships and a quarter (26%) said they are experiencing increased financial insecurity (Table 1).
Six in 10 not offered any form of personalised healthcare
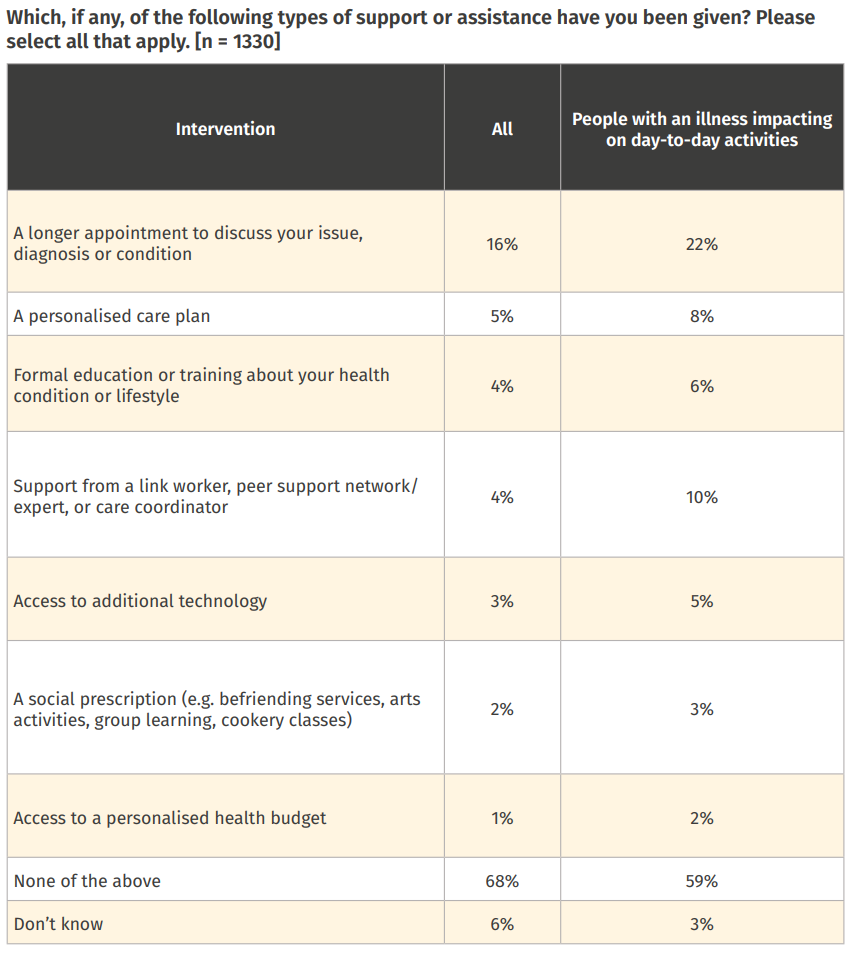
The survey also found that people are not received personalised, preventative interventions, despite NHS commitments. In the survey, people with an illness impacting day-to-day activities were offered:
- A long appointment to discuss their health concern
- A personalised care plan
- Formal education or training about their health conditions or lifestyle
- Support from a link worker, peer support network/expert or care coordinator
- Access to additional technology
- A social prescription
- Access to a personalised health budget.
In total, six in 10 (59%) people with an illness said they had not been offered a single one of these services. This rose to nearly seven in 10 (68%) when people without an illness were included (Table 2).
Only 22% had been offered a longer appointed, 8% a personalised care plan, 6% education about their health condition and 5% additional technology. These are all simple, extra steps that could drastically improve healthy life expectancy, which very few people are being offered access to.
A focus on prevention
The IPPR is now calling for a shift towards providing more individualised healthcare with a focus on preventative efforts. However, they say doing so will require some “fundamental changes in how we approach, fund, and locate healthcare”. This includes:
- A new focus on healthy life expectancy. The think tank suggests the government legislates a 30-year mission to make UK healthy life expectancy the highest in the world.
- A shift to community care, with more services provided in communities and homes (including mobile screening services and health checks).
- A new ‘what works’ centre to create more of a focus on prevention and early diagnosis. A Health Creation Fund would help the government to strategically invest in implementing evidence and new initiatives.
- Rebalancing funding with a greater focus on primary, community, mental health and public health to ‘futureproof’ health and social care services.
Economic case for investment in NHS is “inarguable”
Matthew Taylor, chief executive of NHS Confederation says the survey “bears out the consequences” of an overburdened healthcare system, and says it is clear that demand “has long outstripped supply”.
With this in mind, Mr Taylor says the economic case for investment is “inarguable”, and urges the government to act on the recommendations laid out in the report.
“Not only does every £1 of NHS investment result in a £4 return for the economy but can help prevent patients facing potentially ruinous financial insecurity, by helping them access care faster,” he said.
He also agrees that prevention is key to tackling health inequalities, as well as identifying and tackling the drivers for ill health.
“Keeping people out of hospital and living healthier lives will save money, reduce pressure on services, be better for population health, and improve the prosperity of individuals,” he said.


