Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Alcohol misuse is undeniably a cause of significant morbidity and mortality across all age groups in the UK, with more people dying from alcohol related causes in 2004 than from breast cancer, cervical cancer and MRSA combined.1
While media attention and public health initiatives, such as the Government’s alcohol strategy “Safe. Sensible. Social”, target the young so-called “binge” drinkers,2 the elderly are particularly vulnerable both to excess alcohol consumption and its physiological effects and consequences. A growing literature base suggests we are underestimating and misdiagnosing alcohol problems amongst the elderly,3 with the Royal College of Physicians suggesting 60% of elderly people admitted to hospital with common presentations such as confusion, falls, recurrent chest infections and heart failure may have unrecognised alcohol problems.4
While accurate numbers are difficult to assess for many reasons, it remains reasonable to suggest that we will see an increase in absolute numbers of elderly alcohol misusers as the population ages—what has come to be seen by some as a “silent epidemic”.5–7 This will undoubtedly represent a burden and challenge for healthcare professionals across the NHS, spanning both primary care and hospital services. The estimated annual direct financial cost of alcohol harm alone in 2006 was calculated to be £2.7billion.8
Prevalence of alcohol misuse
The term “alcohol misuse” broadly covers the following two groups.
- Hazardous/harmful drinkers—people who drink more than the recommended limit, at a level believed to cause physiological harm
- “Alcohol dependence”—long-term excessive consumption of alcohol that has led to a physiological dependence and compulsion to drink that provokes symptoms upon withdrawal.
Differences in the definitions for each of these groups exist throughout the literature, and therefore comparable data is difficult to find. Indeed, an editorial published in the British Journal of Psychiatry in 2008 stated: “Harmful use of alcohol is a variable and non-specific term, encompassing various patterns of excess drinking leading to physical, psychological and other indirect impairment”.6
A unit of alcohol is consistently defined as 8mg or 10ml of pure alcohol.9 For a long time, healthy drinking limits have been set at fewer than 21 units a week for males and 14 units a week for females. However, difficulties and inaccuracies in calculating personal weekly alcohol consumption in this way have led to a simplification of the definition. Current Government recommendations are that adult men should not regularly drink more than 3–4 units a day and adult women should not drink more than 2–3 units a day.9 Consistent drinking above these limits has been proven to significantly increase the risk of ill health.10
However questions continue to be raised as to whether these indices are readily applicable to elderly individuals, in whom the physiology of ageing can be seen to reduce tolerance to alcohol.11,12 National annual figures formulated by the Office for National Statistics may thus be seen to be underestimating the level of problem drinkers in the elderly population.13 Bearing this caveat in mind, the 2009 report still suggests that individuals aged 65 years or over were more likely than any other age group to have drunk on every day of the previous week (22% men, 12% women), and rates of drinking above the recommended limits was largely comparable between age groups—worrying in itself.
Further evidence of the presence of “undetected” elderly problem drinkers in the community comes from admission data. Alcohol-related hospital admissions for people in England over 65 years of age showed a huge increase from 197,584 in 2002 to 323,595 in 2007—a rise of over 30%.14
Classification of alcohol misuse
The Institute of Alcohol Studies identifies three types of elderly drinkers:15
- Early-onset drinkers or “survivors”: people who have a continuing problem with alcohol consumption from earlier life. It is thought these represent two-thirds of elderly problem drinkers
- Late-onset drinkers or “reactors”. People who develop problematic drinking habits later in life, often in response to traumatic life events such as the death of a loved one, loneliness, chronic pain, insomnia or retirement
- Intermittent or binge drinkers.
Elderly people who use alcohol occasionally and sometimes drink to excess. It is thought that both the late onset and the intermittent or binge drinkers have a high chance of managing their alcohol problems if given access to appropriate treatment, such as counselling and general support. Hence, patterns of alcohol use in this age group could be seen to be more varied than in younger age groups.
Simple alcohol histories may not identify “survivors”, illustrating a need to consider an approach that takes account of lifelong alcohol history, much in the same way as we assess smoking in “pack years”. Healthcare professionals in the community may also become involved in patient care at the time of a traumatic life event when vigilance to the potential for “reactive” drinking is of particular importance.
Vulnerability to alcohol related harm
As already mentioned, physiological changes in older people could mean that lower levels of alcohol consumption will cause harm. Normal ageing can result in a decreased body water-to-fat ratio as well as decreased hepatic function and blood flow, each decreasing the body’s alcohol tolerance. 4,11–12 Additionally, existing co-morbidities and polypharmacy can conflict and interact with alcohol. Small deficits, such as those in baseline mobility as well as sensory and cognitive deficits for example, are aggravated by alcohol misuse, resulting in an increased likelihood of admission due to falls or confusion.
It is also worth considering the psychological and social factors that could explain why elderly people turn to alcohol, or in other words explain the group of “reactive” drinkers. Loss – of loved ones, of vocation, of status and of independence – could be seen to be major contributors. Studies investigating patterns of alcohol use in the elderly have found that sociodemographic factors associated with unhealthy use of alcohol include male gender,15 social isolation, and being divorced, separated or single.16–18 In many studies, perhaps unsurprisingly, heavy drinking was positively associated with symptoms of depression and anxiety,19,20 although causality is difficult to infer. Knowledge of these “risk factors” could help target and direct screening and interventions to vulnerable people to reduce at-risk drinking in the future.
Diagnosing alcohol misuse
The health-related harm caused by alcohol is well documented; few healthcare professionals would struggle to identify patterns of causation in cases of liver cirrhosis and, more recently, in cardiovascular conditions. Links between alcohol misuse and cancers of the oropharynx, larynx and oesophagus are now being proven as data begins to suggest a causal role for alcohol in rectal and breast cancers.21 Naturally, identifying unhealthy alcohol use in these patient groups could be seen as being too late; however, it nevertheless highlights the importance of considering alcohol history to assist prevention of secondary tumours.
Complaints of falls, incontinence, poor nutrition, self-neglect and confusion can all conceal histories of unhealthy alcohol use in older people. Given the varied presentations, identification of these cases requires healthcare professionals to be vigilant and maintain a high level of suspicion.
Increasing opportunities for diagnosis, alcohol history is classically included in the social history asked in all medical admission clerkings, and forms part of the “lifestyle” questions asked and documented across most GP record systems. However, research has shown that these are poorly completed.21,22 Indeed, only 60% of respondents to the Royal College of Physicians and Royal College of Nursing survey of alcohol services, published in March 2009, confirmed that they routinely screen for alcohol related problems on admission.24
Healthcare professionals may have a lower degree of suspicion of alcohol misuse in the elderly age group,25 decreasing this figure further. Within primary care, it has been suggested that time constraints lead to preferential/ prioritised assessment of what seem “more urgent” health needs in the elderly.4
When they are assessed, alcohol histories can be problematic in elderly patients. Cognitive impairment and ignorance of the alcohol unit system may lead to underestimation of alcohol intake. Elderly patients may also have a generational reluctance to disclose and discuss their intake.25 It has been suggested that relatives may wish to hide evidence of alcohol misuse by elderly people in their family to avoid embarrassment. This social stigma, combined with preconceptions among healthcare professionals, poses challenges to the management of alcohol misuse in older people. A comprehensive BMJ review discussed the concept of “therapeutic nihilism”, where perceptions that alcohol use disorders are ‘understandable’ in the context of poor physical and mental health in the elderly can lead to delays in referral.25
Screening tools
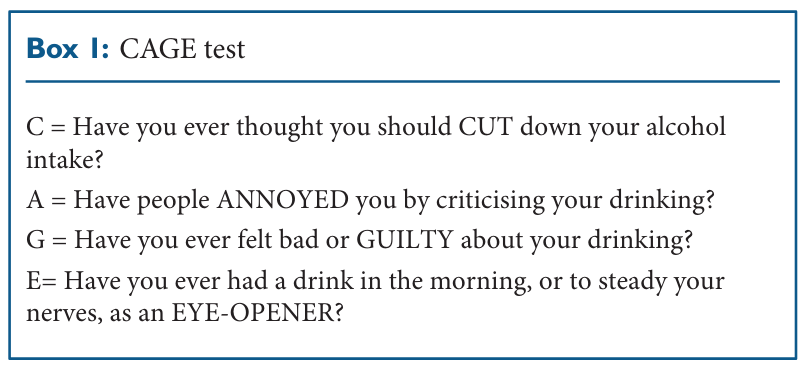
A number of other screening tools and biochemical tests are also used to examine alcohol use. Tools that have been piloted include the CAGE (Cut Down, Annoyed, Guilty and Eye Opener) questionnaire, the geriatric version of the Michigan Alcohol Screening Test (MAST-G), the Alcohol Use Disorders Identification Test (AUDIT), the Fast Alcohol Screening Test (FAST) and the Paddington Alcohol Test (PAT).26–29 Perhaps the best known is the CAGE questionnaire (box 1).
An acronym of its four questions, CAGE allows quick screening of individuals at risk. While not diagnostic, a positive response to two or more questions “should alert the interviewer to the high likelihood of the presence of alcoholism”,27 and provoke further questioning and investigation.
However, these screening tools are unvalidated in the elderly population,29 whose patterns of drinking may differ from that in younger age groups, and they tend to solely assess current intake of alcohol. As already suggested, it may be particularly appropriate to investigate lifetime alcohol consumption in elderly patients. Biochemical tests (such as liver function tests [LFTs], gammaglutamyl transpeptidase [gamma GT] and mean corpuscular volume [MCV] ) may lend weight to suspicions of unhealthy alcohol intake but they are also less specific in elderly patients due to common co-morbidities, such as macrocytic anaemia secondary to pernicious anaemia.
Managing alcohol misuse
Management of alcohol misuse can be divided into two broad situations: acute pharmacological management of “crises” including detoxification, and chronic management of damaging alcohol use, which includes both pharmacological, prophylactic measures and psychological/ behavioural interventions.
Acute care
As already mentioned, fewer elderly patients may present with acute alcohol related “crises”. However, we should consider alcohol withdrawal as a trigger in cases of “acute delirium”. SIGN guidelines exist for the pharmacological management of alcohol withdrawal in adults,30 and NICE guidelines for detoxification in “adults and young people” are scheduled for publication this June. According to SIGN guidance, treatment of alcohol withdrawal in adults should consider the following:
- Thiamine repletion to prevent Korsakoff’s syndrome and Wernicke’s encephalopathy, with either i.v. “Pabrinex” (i.m. in the community) or oral supplementation
- Benzodiazepine (classically chlordiazepoxide) to protect against withdrawal seizures.30
While health professionals commonly believe alcohol withdrawal symptoms may be more severe in elderly patients, this has not been proven. SIGN indeed suggests, “there is no difference between alcohol withdrawal symptoms in the elderly, or the amount/type of benzodiazepine required for detoxification”.
However, as the physiological changes associated with ageing can alter the pharmacokinetic profile of alcohol, the likelihood of altered metabolism and accumulation of benzodiazepines needs to be considered. Studies reviewing benzodiazepine use in elderly patients undergoing withdrawal have largely concluded that, while short acting benzodiazepines may reduce the risk of excess sedation and accumulation associated with long-acting benzodiazepines, they may be less effective at preventing seizures. Consequently, the SIGN guidance currently states: “Provided attention is paid to any acute or chronic physical illness, elderly patients should be managed in the same way as adults”. Given the high degree of medical comorbidity, however, authors across the literature recommend admission.
Chronic care
Pharmacological measures to prevent alcohol-related harm include long-term thiamine supplementation, and, once a period of abstinence has been achieved, medications in addition to psychosocial intervention to prevent relapse. Acamprosate and disulfiram are both licensed for use in adults (where naltrexone is not), but little evidence supports their use in the elderly. Cognitive impairment and lack of supervision may be concerns with disulfiram, which can induce potentially severe physiological reactions when used with alcohol.
“Chronic” management of alcohol misuse largely focuses on behavioural/psychological measures that address patients’ individual reasons for drinking. In the primary care setting, these include information, advice, education, counselling, and motivational interviewing. “Brief intervention programmes” such as these have been consistently effective in maintaining abstinence and reducing alcohol consumption in adults.21,29,31
A Cochrane review suggests the use of three to four standard consultations, of five to 10 minutes’ duration, to offer: information on alcohol-related harm, advice on identifying high-risk situations for drinking; coping strategies and an opportunity to develop a personalised plan to reduce alcohol intake.31 It could be difficult to apply this to elderly patients, who are at higher risk of social isolation and cognitive impairment but, encouragingly, if access problems can be overcome, the older age group can derive more benefit from such services.32
Problems with provision
Worryingly, over 75% of respondents to the joint Royal College of Physicians and Royal College of Nursing survey classified NHS alcohol services inadequate or very inadequate.24 Hospitals and A&E departments have started recruiting alcohol specialist nursing teams to address problems, provide advice and follow-up patients, but further ways of supporting GPs and community health services are needed.
Conclusion
Misuse of alcohol amongst the elderly population is increasing, with different patterns of alcohol use and existing co-morbidities potentially clouding diagnosis. Recommended limits to alcohol intake need to be redefined for the elderly population in line with ageing physiology, and separate screening tools should be validated for older patients. Healthcare professionals across primary, secondary and tertiary NHS facilities should be vigilant to the role of alcohol in common presentations in older people, and provide early and effective intervention to prevent harm following opportunistic screening.
We have no conflict of interest
Dr E J Williams, Foundation year 2 doctor, Gloucester Royal Hospital
Dr P Medcalf, Consultant in Acute and Old Age Medicine, Gloucester Royal Hospital
References
- Office of National Statistics. Mortality statistics: Deaths registered in England and Wales. 2006. http://tiny.cc/n1ii8 (accessed 11 May 2010)
- Department of Health. Sensible. Social. The next steps in the national alcohol strategy London: http://tiny.cc/pv6y5 (accessed 11 May 2010)
- Khan N, Davis P, Wilkins TJ, et al. Drinking patterns among older people in the community: hidden from medical attention? NZ Medical Journal 2002; 115: 72–75
- Institute of Alcohol Studies. Factsheet: Alcohol & the Elderly. Jan 2009. http://tiny.cc/hz1ij (accessed 11 May 2010)
- Lister, H. Growing problem of alcohol abuse among elderly uncovered. July 2009. The Times. Accessed online: http://tiny.cc/ pv6y5e (accessed 11 May 2010)
- Gupta S, Warner J. Alcoholrelated dementia: a 21st century silent epidemic? British Journal of Psychiatry 2008; 193: 351–353
- Knauer C. Geriatric Alcohol abuse: a national epidemic. Geriatric Nursing. 2003; 24(3):152–54
- Alcohol Learning Centre. The cost of alcohol harm to the NHS in England –an update to the Cabinet 2008. http://tiny.cc/dtrbg (accessed 11 May 2010) 9. The NHS Information Centre. Statistics on Alcohol, England 2009.
- Department of health website. Accessed online. http://tiny.cc/ a5c09 (accessed 11 May 2010)
- Reid MC, Anderson PA. Geriatric substance use disorders. Med Clin North America 1997 81: 999–1016
- Tupler LA, Hege S, Ellinwood EH. Alcohol pharmacodynamics in young-elderly adults contrasted with young and middle aged subjects. Psychopharmacology 1995; 118(4): 460–70
- Office of National Statistics. General Lifestyle Survey (formerly General household survey). “Smoking and drinking amongst adults” 2008. http://tiny.cc/rxvpy (accessed 11 May 2010)
- Primarolo D (Rt Hon). Response to parliamentary question. House of Commons Hansard. Written answer. “Alcoholic drinks: Elderly”. 26 February 2009. http:// tiny.cc/lp2e7 (accessed 11 May 2010)
- Saunders PA, Copeland JR, Dewey ME, et al. Heavy drinking as a risk factor for depression and dementia in elderly men. Findings from the Liverpool longitudinal community study. British Journal of Psychiatry 1991; 159: 213–6
- Bristow MF, Clare AW. Prevalence and characteristic of at risk drinkers among elderly acute medical inpatients. British Journal of Addiction 1992; 87: 291–4
- Ganry O, Joly J, Queval MP, Dubreuil A. Prevalence of alcohol problems among elderly patients in a university hospital. Addiction. 2000; 95: 107–13
- Ekerdt DJ, DeLabry LO, Glynn RJ, Davis R. Change in drinking behaviours with retirement: findings from the normative ageing study. Journal Studies Alcohol 1989. 50: 347–53
- Merrick EL, Horgan CM, Hodgkin D, et al. Unhealthy drinking patterns in older adults: prevalence and associated characteristics. Journal American Geriatric Society 2008. 56(2): 214– 23
- Kirchner JE, Zubritsky C, Cody M, Coakley E, et al. Alcohol Consumption among older adults in primary care. Journal of General Internal Medicine 2007; 22(1): 92–97
- NICE/Health development agency. Prevention and reduction of alcohol misuse. Evidence briefing summary. 2nd edition, March 2005. London: HAD. March 2005. http://tiny.cc/lp2e7 (accessed 11 May 2010)
- Rowland N, Maynard A, Beveridge A, et al. Doctors have no time for alcohol screening. BMJ 1987; 295: 95–6
- Thompson D. Alcohol histories taken from elderly people. BMJ 1994; 308: 722
- Royal College of Physicians and Royal College of Nursing Survey on Alcohol Treatment Services. March 2009. http://tiny.cc/q9psi (accessed 11 May 2010)
- O’Connell H, Chin A-V, Cunningham C, Lawlor B. Clinical Review. Alcohol use disorders in elderly people—redefining and age old problem in old age. BMJ 2003; 327: 664–7
- Johnson-Greene D, McCaul ME, Roger P. Screening for hazardous drinking using the Michigan Alcohol Screening test – geriatric version in elderly persons with acute cerebrovascular accidents. Alcoholism. Clin and Experimental Research 2009; 33(9):1555–61
- Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA 1984. 252: 1905–7.
- Saunders JB. Development of the alcohol use disorders identification test (AUDIT). Addiction 1993; 88 791–804
- Culberson JW. Alcohol use in the elderly: beyond the CAGE. Part two: Screening instruments and treatment strategies. Geriatrics 2006. 61(11): 20–6
- The management of harmful drinking and alcohol dependence in primary care. Scottish intercollegiate guidelines network. 2003, guideline number 74. http:// tiny.cc/r3m5u (accessed 11 May 2010)
- Kaner E, Beyer F, Dickinson H, et.al. Effectiveness of brief alcohol related interventions in primary care populations. Cochrane Database of Systematic Reviews 2007.
- Kofoed LL, Tolson RL, Atkinson RM, Toth RL, Turner JA. Treatment compliance of older alcoholics: An elder specific approach is superior to “mainstreaming”. J Stud Alcohol 1987; 48: 47
- Huibers MJH, Buerskens AJHM, Bleijenberg G, Van Schayk CP. The effectiveness of psychological interventions delivered by general practitioners. The Cochrane Database of Systematic Reviews. Issue 2. 2003


