Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Hypokalaemia is one of the most common electrolyte abnormalities encountered in clinical practice. More than 20% of patients in hospital have hypokalaemia, when defined as a serum potassium level of less than 3·6 mmol/l.1 Moderate hypokalaemia is defined as a serum level of 2·5–3 mmol/l while severe hypokalaemia is less than 2·5 mmol/l.2
Different risk thresholds are reported in at-risk patients and, in the situation of acute myocardial infarction, patients with potassium concentrations below 4·0 mmol/l were reported to be at significantly increased risk of ventricular arrhythmias.3 Because potassium is a major intracellular cation, the tissues most severely affected by potassium imbalance are muscle and renal tubular cells.

Depletional hypokalaemia
Renal loss
The most common cause of hypokalaemia in primary care is use of loop or thiazide diuretics, which is more common in those with predisposing disease such as heart and liver disease.4,5 The next most common cause is hyperaldosteronism, due to heart failure or liver disease. High normal serum sodium and normal or low potassium are typically seen in primary hyperaldosteronism (Conn’s syndrome), which should be considered in patients with refractory hypertension.
Rarer causes include the renal disorders Liddle’s syndrome and Bartter’s syndrome and renal tubular acidosis (types 1 and 2). When the cause of hypokalaemia is unclear, a urinary potassium measurement will help to identify renal loss.6 Abuse of diuretics or alkalis such as milk of magnesia should be considered. Ectopic production of ACTH may cause rapid onset and severe hypokalaemia. Potential causes are summarised in Box 1.
Extra-renal loss
Causes include inadequate ingestion due to fasting or the “tea and toast” diet of elderly people. Loss from the lower gastrointestinal tract is common and usually associated with hyperchloraemic acidosis due to bicarbonate loss. Causes to consider include laxative abuse, villous adenomas, secretory small-bowel diarrhoea and inflammatory bowel disease. Vomiting produces hypokalaemia if prolonged, or in infants or frail elderly patients as a result of alkalosis. Most of these causes should be clinically apparent.
Redistributional hypokalaemia
Redistribution from the extracellular to the intracellular compartment may occur acutely in alkalosis, as a result of administration of insulin in ketoacidosis, and in the rare situation of familial and sporadic hypokalaemic periodic paralysis. A combination of depletion and redistribution can occur in catecholamine release or administration of β-mimetics.3 Redistribution also occurs in refeeding after starvation, in stress due to surgery or severe illness, and in the acute treatment of pernicious anaemia.
Signs and symptoms of hypokalaemia
Manifestations of hypokalaemia include generalised muscle weakness, paralytic ileus, and cardiac arrhythmias (atrial tachycardia with or without block, atrioventricular dissociation ventricular tachycardia, and ventricular fibrillation). In severe untreated hypokalaemia, myopathy may progress to rhabdomyolysis, myoglobinuria, and acute renal failure. Such complications are most often seen in hypokalaemia secondary to alcoholism.3 A list of classical signs, symptoms and findings is shown in Box 2.
ECG abnormalities
Hyperpolarisation of the excitable membranes occurs in hypokalaemia. This increases the threshold for initiation of an action potential and interferes with its termination. Apart from arrhythmia, ECG findings are reported with increasing frequency and severity at serum concentrations of 3·0 mmol/l and below.4 Typical electrocardiographic changes include flat or inverted T waves, ST-segment depression, and prominent U waves.
Hypomagnesaemia
Gastrointestinal potassium loss and diuretic-induced hypokalaemia both commonly coexist with hypomagnesaemia, which may predispose to or aggravate arrhythmias and render potassium-replacement ineffective.4,7
Management of hypokalaemia
Compensation for potassium losses is necessary for patients who:
- Take digoxin or other antiarrhythmic medicine that can deplete potassium and induce arrhythmias.8
 Patients at risk of arrhythmias include those on digoxin and those with cardiac disease (ischaemia, heart failure or left ventricular hypertrophy).4 The arrhythmogenic potential of digoxin has been shown to be enhanced by hypokalaemia in patients with heart failure.3,5 Several observational studies have reported adverse outcomes for patients with hypokalaemia who were taking digoxin. Potassium supplementation has been recommended for patients with serum potassium concentrations at a higher threshold (3·7 mmol/l) to maintain serum potassium concentrations at 4·0 mmol/l3 and 4·5–5 mmol/l.5
Patients at risk of arrhythmias include those on digoxin and those with cardiac disease (ischaemia, heart failure or left ventricular hypertrophy).4 The arrhythmogenic potential of digoxin has been shown to be enhanced by hypokalaemia in patients with heart failure.3,5 Several observational studies have reported adverse outcomes for patients with hypokalaemia who were taking digoxin. Potassium supplementation has been recommended for patients with serum potassium concentrations at a higher threshold (3·7 mmol/l) to maintain serum potassium concentrations at 4·0 mmol/l3 and 4·5–5 mmol/l.5
- Have excessive potassium loss (e.g., from chronic diarrhoea, fistulae)8
Diarrhoea is a common underlying cause of hypokalaemia and needs to be considered in any investigations.4 Likewise, any patients with a history of a fistula need to be investigated as to whether this is causing loss of potassium.
Preventing hypokalaemia
- Consider dietary advice regarding potassium–rich food.8
The hypokalaemic patient’s nutritional status should be considered as well as their dietary intake. Increasing dietary potassium is the most straightforward means of enhancing potassium intake, ideally using potassium-rich foods and supplementation. Dietary sources of potassium include: coffee, nuts, tomatoes, bananas and chocolate (Box 3). Tomato juice contains approximately 8 mmol in a standard 100 ml glass.4 However, dietary potassium is almost entirely coupled with phosphate, rather than with chloride; therefore, it is not effective in correcting potassium loss that is associated with chloride depletion, such as in diuretic therapy, vomiting, and nasogastric drainage.3,9
- Potassium-sparing diuretics are preferable to long-term potassium salts when large doses of diuretics are used to treat oedema
When diuretic therapy is necessary, potassium balance should be protected by using low-dose diuretics and by using diuretics in combination with drugs that have the potential for sparing potassium (such as β-blockers, potassium-sparing diuretics, ACE inhibitors, or angiotensin receptor blockers).3
In the UK, potassium-sparing diuretics are recommended as the preference for patients on potassium-lowering diuretics.10 A systematic review has suggested that virtually all patients with congestive heart failure should receive potassium supplementation, a potassium sparing diuretic, or an ACE inhibitor.5 A further review found a clear dose-response effect on decreasing serum potassium for the diuretics hydrochlorothiazide, chlorthalidone and cyclopenthiazide in hypertensive patients.11
One review of randomised trials found a doubling in mortality rate in patients receiving thiazide versus potassium-sparing diuretics in hypertensive patients.11 Several authors recommend routine potassium supplementation or potassium-sparing agents in patients receiving diuretics.3 The Multiple Risk Factor Intervention Trial12 found that use of non-potassium-sparing diuretics was associated with an increased risk of sudden death in men with baseline ECG abnormalities. In the Swedish Trial in Old Patients with Hypertension11,13 treatment with atenolol or a diuretic combination of amiloride and hydrochlorothiazide reduced the incidence of sudden death compared with placebo (rate 0·33, 95% CI 0·08–1·10).

- Reduce the dose of potassium supplements in renal failure or elderly patients.8
Patients with acute renal failure are at risk of having true rather than spurious hyperkalaemia. Hyperkalaemia in chronic kidney disease may be precipitated by small changes in diet, therapeutic drugs, changes in eGFR, new infection, or new diabetic ketoacidosis. Use of low salt-type salt substitutes has also been implicated in life-threatening hyperkalaemia in renal failure.4,14 A review has shown that people older than 70 years are at greater risk from severe hyperkalaemia.4
Established potassium depletion
- Oral doses of 70–100 mmol/ day may be required for several days for plasma potassium of 2·5–3·5 mmol/l.8
Potassium supplementation of 40–120 mmol/day is recommended by a review depending on the level of deficiency and urgency.4 This should be in conjunction with regular potassium monitoring, weekly to several times weekly depending on the deficiency. Target concentrations of up to 4·5 mmol/l and above are appropriate in higher risk patients.4 A further review suggested that a dose of 20 mmol/d of potassium in oral form is generally sufficient for the prevention of hypokalaemia, and 40 to 100 mmol/d sufficient for its treatment.
- Give potassium salts as liquid or well diluted soluble tablets rather than slow release preparations.8
The British National Formulary recommends liquid-based or effervescent preparations as first-line potassium salt treatment.10 However, one review reports liquid potassium chloride as less well tolerated by some patients and that tablet formulations may be superior, partly for compliance reasons.3,15 Liquid forms may be less expensive but they have a strong, unpleasant taste and often are not well tolerated.3 In a study of more than 2000 patients, the worst adherence ratios were observed in patients who were treated with liquid potassium supplements, which the authors speculated may have been due to increased side-effects, poor taste, and the inconvenience of liquid supplements.15
Ulcerations of the small bowel have been reported after the administration of entericcoated potassium chloride tablets. Although slow-release tablets have been associated with gastrointestinal tract ulcerations and bleeding, the risk of these complications is low and seems to be lowest with microencapsulated preparations.9 Wax matrix-based formulations (such as Slow-KH) have been associated with cases of gastric erosions in some people.3 Effervescent tablet preparations, if well tolerated, would appear to represent a compromise between speed of action, dose convenience, and gastric safety (table 1).3
- For severe depletion i.e., plasma potassium <2·5mmol/l— consider using premixed bags of iv fluids containing potassium chloride. The peripheral infusion rate not to exceed 10 mmol/hour.8
In general, oral therapy is the preferred route for potassium repletion because it is easy to administer, safe, inexpensive, and readily absorbed from the gastrointestinal tract. For patients who have severe hypokalaemia and are symptomatic, both intravenous and oral replacement are necessary. If the potassium level is less than 2·5 mmol/l, intravenous potassium should be given.16 One review advocates that patients should receive no more than 20 mmol/h iv to avoid potential deleterious effects on the cardiac conduction system.
Potassium solutions should never be given as an intravenous push and should be administered as a dilute solution. A paper has recommended that if rapid (>10 mmol/h)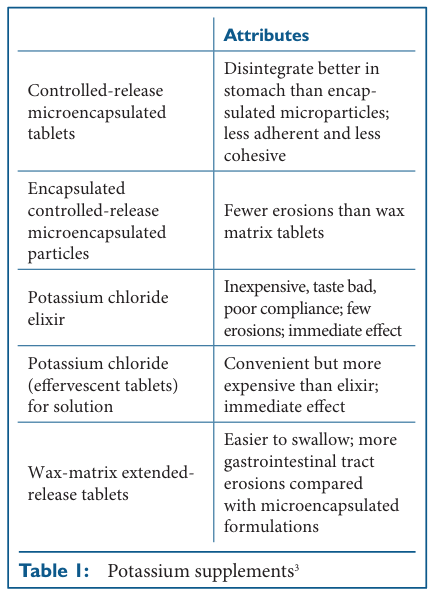 potassium administration is given intravenously, cardiac monitoring in an intensive care unit is advisable.2 Ready-mixed infusion solutions should be used when possible; alternatively, potassium chloride concentrate, as ampoules containing 1·5 g (K+ 20 mmol) in 10 ml, is thoroughly mixed with 500 ml of sodium chloride 0·9% intravenous infusion and given slowly over 2–3 hours, with specialist advice and ECG monitoring in difficult cases.10 Higher concentrations of intravenous potassium are damaging to small peripheral veins, resulting in pain and sclerosis.16,17
potassium administration is given intravenously, cardiac monitoring in an intensive care unit is advisable.2 Ready-mixed infusion solutions should be used when possible; alternatively, potassium chloride concentrate, as ampoules containing 1·5 g (K+ 20 mmol) in 10 ml, is thoroughly mixed with 500 ml of sodium chloride 0·9% intravenous infusion and given slowly over 2–3 hours, with specialist advice and ECG monitoring in difficult cases.10 Higher concentrations of intravenous potassium are damaging to small peripheral veins, resulting in pain and sclerosis.16,17
Conclusion
Compensation for potassium losses is necessary for patients who are taking digoxin or other anti-arrhythmic medicines where potassium depletion may induce arrhythmias; or those who have excessive potassium loss e.g., chronic diarrhoea, or fistulae. Consider giving dietary advice regarding potassium–rich foods. Potassium sparing diuretics are preferable to chronic administration of potassium salts when large doses of diuretics are used to treat oedema.
Reduce the dose of potassium supplements in renal failure or elderly patients. Oral doses of 70–100 mmol/day may be required for several days for plasma potassium of 2·5–3·5 mmol/l. Give potassium salts as liquid or well diluted soluble tablets rather than slow-release preparations. For severe depletion (i.e., plasma potassium less than 2·5 mmol/l), consider iv therapy using premixed bags of iv fluids containing potassium chloride. The peripheral infusion rate should not exceed 10 mmol/ hour.
Dr Anthony Crosse, 88 Bayside Crescent, Sutton, Dublin 13, Ireland.
References
- Paice BJ, Paterson KR, OnyangaOmara F et al. Record linkage study of hypokalaemia in hospitalized patients. Postgrad Med J 1986; 62: 187–91
- Garth D, MD, Hypokalemia. http:// www.emedicine.com/emerg/ topic273.htm (accessed 4 August 2008)
- Cohn J N, Kowey P R, Whelton P K, et al. New Guidelines for potassium replacement in Clinical Practice. A contemporary review by the National Council on potassium in clinical practice. Arch Intern Med 2000;160: 2429–36
- Smellie WSA, Shaw N, Bowlees, et al. Best practice in primary care pathology: review 9. J Clin Pathol 2007; 60: 966–74 5. Leier CV, Dei Cas L, Metra M. Clinical relevance and management of the major electrolyte abnormalities in congestive heart failure: hyponatraemia, hypokalaemia and hypomagnesaemia. Am Heart J 1994; 128: 564–73
- Lin S-H, Lin Y-F, Chen D-T, et al. Laboratory tests to determine the cause of hypokalaemia and paralysis. Arch Int Med 2004;164: 1561–66
- Whang R, Whang DD, Ryan MP. Refractory potassium repletion: a consequence of magnesium deficiency. Arch Intern Med 1992; 152: 40–45
- The Royal Liverpool University Hospitals: Broadgreen and Liverpool Formulary and Prescribing Guidelines 2007–08. 244–49
- Gennari FJ. Hypokalemia. N Engl J Med 1998; 339: 451–58
- British National Formulary. Section 9.2.1.1. Oral potassium; 2005: 471– 72
- Grobbee DE, Hoes AW. Nonpotassium-sparing diuretics and risk of sudden cardiac death. J Hypertens 1995; 13: 1539–45.
- Multiple Risk Factor Intervention Trial Research Group: Multiple Risk Factor Intervention Trial. Risk factor changes and mortality results. JAMA 1982; 248: 1465–77
- Dahlof B, Lindholm LH, Hansson L et al. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOPHypertension). Lancet 1991; 338: 1281–85
- Mandal AK. Hypokalemia and hyperkalemia. Med Clin North Am 1997; 81: 611–39
- Halpern MT, Irwin DE, Brown HE, et al. Patient adherence to prescribed potassium supplement therapy. Clin Ther 1993; 15: 1133– 45
- Sterns RH, Feig PU, Pring M, et al: disposition of intravenous potassium in anuric man: a kinetic analysis. Kidney Int 1979; 15: 651– 60
- Kim GH, Hans JS. Therapeutic approach to hypokalaemia. Nephron 2002: 2(Suppl 1): 28–32


