Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
The UK has an ageing population with a significant burden of frailty and comorbidities. One in five are aged over 65 years old and in 10 years’ time this will have increased to 13 million people, which is 22% of the population. Major comorbidities are highest in older individuals and 9.1 million people in England are projected to be living with major illness.1,2
One in ten older people are also suffering from or are at risk of malnutrition. This results from lack of uptake of nutrition and leads to altered body composition and body cell mass, diminished physical and mental function, and impaired clinical outcome from disease.3
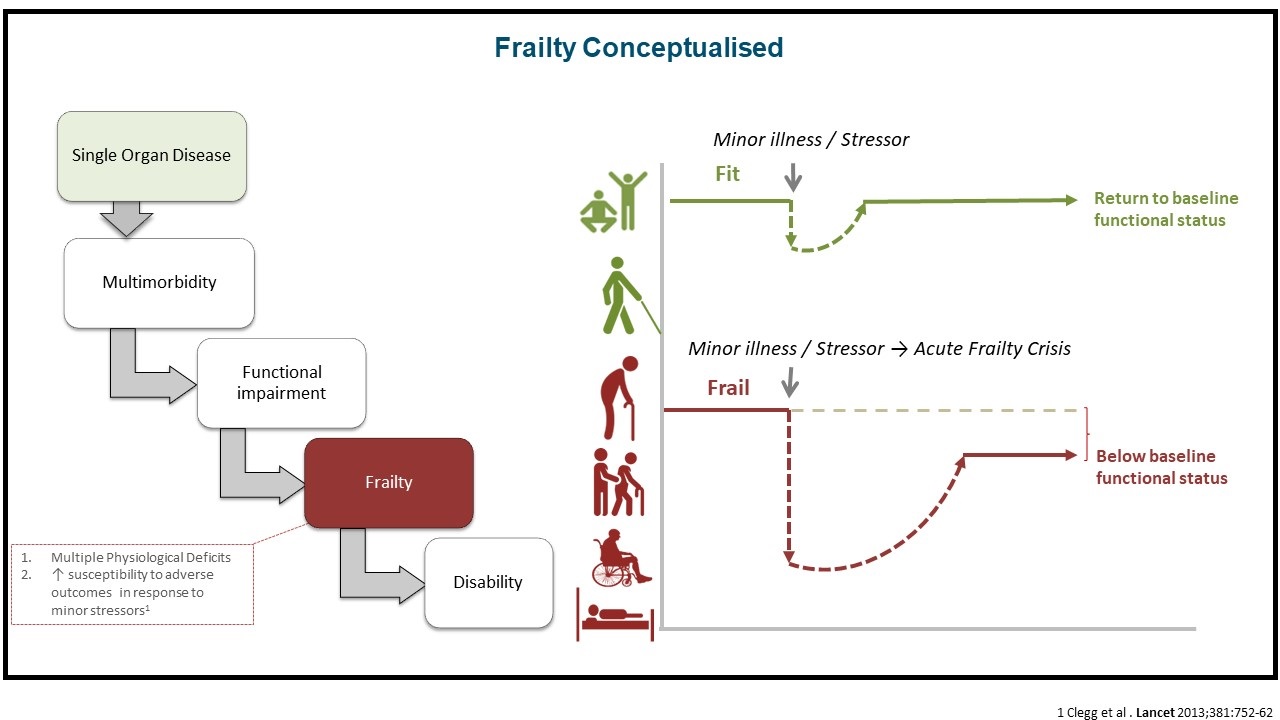
Malnutrition drives progression of frailty, which is defined as multiple physiological deficits and increased susceptibility to adverse outcomes in response to minor stressors.4 An acute frailty crisis can lead to an increased risk of falls, delirium, adverse drug effects, mobility and functional decline, as well as increased personal and social needs.
Multiple biological processes have been implicated in the development of frailty, including alterations in brain functions, dysregulation in endocrine systems; metabolic perturbation related to glucose, insulin, micronutrients; end-product/waste retention; oxidative stress; chronic inflammation; vitamin D insufficiency; reproductive hormone deficiency; and immune dysfunction.5 Dynamic changes in these pathologies and subsequent synergism further affect the pace of frailty development and aggravation.
Sarcopenia and frailty
Sarcopenia is characterised by progressive and widespread skeletal muscle loss leading to poor muscle strength and performance. Ageing is a significant risk factor and it is associated with negative health outcomes, such as increased risk of infection, decreased wound healing, difficulty sitting and pressure ulcers, There is also an increased risk of death in severe sarcopenia, usually from pneumonia.6,7
One study found malnutrition was associated with an approximately fourfold higher risk of developing sarcopenia/severe sarcopenia during a four-year follow-up.8
This is is because protein shortfall impairs muscle protein synthesis in old age resulting in sarcopenia and decreased physical function. This can lead to decreased muscle strength and risk of dependence, loss of autonomy, hospital admission and care home admission.
Factors accelerating muscle loss include malnutrition, acute illnesses and comorbidities, decreased activity, smoking, alcohol misuse, periods of immobilisation, and hospital admissions. Sarcopenia and osteoporosis can also occur together, which is known as osteosarcopenia.

Poor muscle health can be diagnosed using screening tools such as SARC‐F, which is a simple five‐item questionnaire based on cardinal features or consequences of sarcopenia, including assessing strength, assistance in walking, rising from a chair, climbing stairs, and falls.9,10
Approximately one third to one half of individuals aged 65 years or older report difficulties related to walking or climbing stairs.11
Comprehensive geriatric assessment (CGA) and use of screening tools such as the Frailty Scale and MUST tool for assessing for malnutrition can also aid in frailty management. In the hospital setting, CGA is effective in reducing mortality and improving independence (still living at home). In the community setting, it can reduce hospital admission and can reduce the risk of readmission in those recently discharged.
For sarcopenia management, there is no specific pharmacological agent in routine clinical practice at present. Potential drugs being investigated may rebalance protein synthesis and degradation, reshape the endocrine system, reduce oxidative stress and promote mitochondrial function, and result in beneficial effects in muscle hypertrophy.
Optimising nutritional intake
Multiple studies have indicated that at least 25-30g of high-quality protein is necessary at each meal to optimally build or maintain muscle in older people and those who are unwell.12
Food fortification is the addition of vitamins and minerals to foods and it plays an important role in improving micronutrient intake.13 Based on the ‘food first’ approach, energy and protein-based fortification is viewed as an effective, well-tolerated, and cost-effective intervention to improve dietary intake of older people.12
Oral nutritional supplements (ONS) are sterile liquids, semi-solids or powders, which provide macro and micronutrients. They can be prescribed in the short-term for acute illnesses or for individuals with chronic conditions. ONS are used when diet alone is insufficient to meet daily nutritional requirements, but they are NOT intended as a food replacement
Many frail older individuals do better with high protein low volume ONS that are better able to meet additional protein and calorie requirement.14
As systematic review and meta-analysis showed a significant reduction in complications with multi-nutrient ONS (mean intake 588 kcal, 22 g/d protein, mainly ready to drink), consumed in the community, including pre and post operatively, for around three months predominantly in older patients (mean age 67 years) with benefits seen across a wide variety of patients groups.15
In conclusion, slowing progression of frailty and sarcopenia can be done with proactive assessment and management through education and increased public health awareness. Healthcare professionals can provide information to patients/carers about loss of muscle mass as well as making patients/carers aware of why a high protein diet is important. They should also communicate the synergistic role for nutrition and exercise.
CGA can also aid in the individualised management of frailty, sarcopenia and malnutrition. Older age is associated with a protein shortfall in diet contributing significantly to poor muscle health (sarcopenia). Therefore it is important to increase the amount of protein in diet, prescribe HP-ONS where indicated. This can be combined with individualised exercise programme, especially resistance exercises, to improve muscle health
Useful resources
- Ageing Better – Raising the bar on strength and balance
- BAPEN – Managing malnutrition
- Royal College of Physician – Falls and frailty fracture audit programme
Dr Sanjay Suman, Consultant Geriatrician and Clinical Director, Medway NHS, Kent
This article is based on a recent webinar and is available to view in our events section
References
-
- Ageing Better responds to new report warning one in five people in England will have a major illness by 2040 | Centre for Ageing Better (ageing-better.org.uk)
- https://www.health.org.uk/news-and-comment/news/25-million-more-people-in-england-projected-to-be-living-with-major-illness-by-2040
- Clin. Nutr. 2015;34:335–340. doi: 10.1016/j.clnu.2015.03.001
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013 Mar 2;381(9868):752-62. doi: 10.1016/S0140-6736(12)62167-9
- Nitta, K., Hanafusa, N., Kawaguchi, Y. et al. Physical function management for elderly dialysis patients: prevention and improvement of frailty and disability. Ren Replace Ther 9, 2 (2023). https://doi.org/10.1186/s41100-023-00459-2
- DOI: 10.3233/OER-170250 https://content.iospress.com/journals/occupational-ergonomics
- https://doi.org/10.1016/j.jamda.2016.04.019
- https://doi.org/10.3390%2Fnu11122883
- Cruz-Jentoft AJ, et al. Age Ageing. 2019;48(1):16-31
- Malmstrom TK, Morley JE. JAMDA. 2013;14:531-532
- https://doi.org/10.2147%2FCIA.S253535
- Malnutrition Pathway. 2021. Managing Adult Malnutrition in the Community. 3rd Edition. Accessed 2022.
- BDA. 2021. Food Fortification. Accessed 2022. 3. Roberts, H.C. The challenge of managing undernutrition in older people with frailty. Nutrients, 2019. 11(4), p.808.
- https://doi.org/10.1016/j.arr.2023.1019
- BAPEN. 2016. Nutritional Support: Oral Nutritional Supplements. Accessed 2022


